Angina
Angina is a common cause of chest pain caused by a reduced supply of blood to the heart muscle which tends to occur during exercise. The reduced blood supply to the heart occurs because the arteries that supply blood to the heart (the coronary arteries) have become narrowed as a result of cholesterol deposited in their walls. This process where the coronary arteries become narrowed is commonly called coronary artery disease. This coronary artery disease then restricts blood flow to your heart so the muscle cells do not receive enough oxygen and nutrients.
There are several treatment options for angina. These include lifestyle modifications, treatment with medication, treating the diseased arteries by stretching the narrowed part of the artery with a balloon and then inserting a stent (percutaneous coronary intervention or PCI) or an operation to bypass the blocked or narrowed arteries (coronary artery bypass surgery or a CABG).
Symptoms of Angina
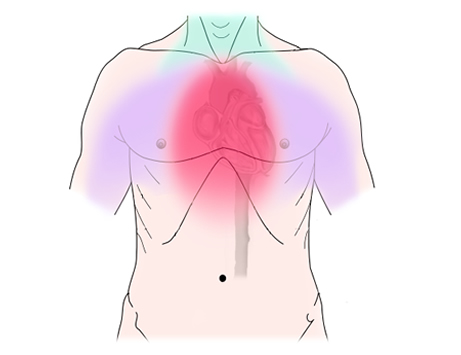
Besides chest pain, which may feel heavy, tight or like a dull ache, you may feel other symptoms at the time of an angina attack. For instance, the pain you feel in your chest may spread down your arms or into your neck, jaw or back. Other symptoms can include:
-
Breathlessness, which is sometimes the only symptom and may occur without a pain in your chest
-
Feeling nauseous
-
Extreme tiredness
-
Feeling dizzy
-
Feeling restless
What triggers an angina attack depends on the type of angina you have. If you have stable exertional angina, exercise or emotional stress is a common trigger. Exercise in the cold weather may bring an attack on earlier. Exercise after eating a large meal may also precipitate symptoms. This occurs because your heart needs to work harder in these situations, but your symptoms should resolve after a few minutes of rest. In unstable angina, there often is no obvious trigger, and symptoms may occur at rest or on minimal exertion.
Risk Factors for Angina
Any factors that make your coronary arteries susceptible to narrowing increases your risk of developing chest discomfort or angina due to reduced coronary blood flow. The following all increase your risk of developing angina:
-
Increasing age
-
A family history of circulatory disease, particularly of a first degree relative
-
High blood pressure
-
High cholesterol, in particular a high level of LDL cholesterol which promotes narrowing of your arteries
-
Diabetes
-
Smoking, as the chemicals in cigarette smoke harm your blood vessels
-
Sedentary lifestyle
Taking steps to change your lifestyle and make sure that you get any contributing medical conditions under good control can help to prevent the development of angina and the progression of the coronary artery disease if you have already developed angina.
Diagnosing Angina
As well as assessing your symptoms and identifying risk factors for coronary artery disease, you will need investigations to confirm the diagnosis of angina and to make an appropriate treatment plan. These include an ECG which will most likely be performed at the time of initial consultation. There are other more specialised tests to determine if the arteries that supply blood to the heart are narrowed and to assess the severity of any narrowings. These split into two categories; non-invasive tests and invasive tests.
Non-invasive tests are tests on the heart which require no more than simple injections of dye or other medications to either speed up or slow down the speed of your heartbeat. These include a CT scan of the heart arteries (where an injection of dye is needed and often an injection to slow down the speed of the heart) and a cardiovascular MRI scan of the heart (where an injection of dye is needed and also injection of a medication to temporarily speed up the heart). The results of these tests can then determine if you have significant narrowings of the arteries of your heart.
If these non-invasive tests show that you are likely to have narrowings in the arteries of your heart then you may be recommended to have a test called a coronary angiogram. You may also be advised to have a coronary angiogram if you have symptoms of angina that are concerning or your risk factor profile for coronary artery disease makes it very likely that you will have developed the disease. This is an invasive test where a small tube (known as a catheter) will be inserted through the artery either at the top of your leg or your wrist around into the heart arteries and pictures of the heart arteries are then taken using dye and x-rays. This test is also needed to plan if you need to have any of your arteries treated by stretching them with a balloon and then inserting a stent (PCI) to keep them open. It is also needed if you then need coronary artery bypass surgery so that the surgeon knows where the narrowings and blockages in your heart arteries are located.
Treating Angina
Management for angina aims to offer symptom relief and to reduce the frequency of further attacks. There are several medications that can be used to treat angina. These include regular medications and also medications that are taken during an attack of angina. Medications that are taken during an attack include nitrate sprays or tablets which are either sprayed or placed under the tongue to relieve your chest pain or other symptoms. Medications which are taken regularly to reduce the frequency of attacks of angina include beta-blockers (eg Atenolol and Bisoprolol), calcium channel blockers (eg Diltiazem, Amlodipine or Verapamil), potassium channel activating agents (eg Nicorandil) and regular nitrates. There are also new treatment options such as Ranolazine and Ivabradine which can be used. The exact combination of treatments will depend on your symptoms and any other medical conditions that you may have.
In addition to medication to specifically treat the angina if you have any medical condition which increases the risk of coronary artery disease (such as high blood pressure of high cholesterol) then this will also need to be treated. In nearly all cases Aspirin or another blood thinning drug (eg Clopidogrel, Prasugrel or Ticlopidine) will be prescibed. These will reduce the risk of further problems with your heart in the future.
In many cases after treatment has been started either percutaneous coronary intervention or coronary artery bypass surgery will also be discussed. This will depend on the exact nature of your symptoms and the number of narrowings or blockages in your heart arteries and the location of these blockages in your arteries.